I'm one of many people with dissociative identity disorder (DID). I lose time, regularly forget pretty important stuff, and I have alters who behave according to their perceptions of the world, not mine. How does that translate to daily life? I mess up - badly and often. As I see it, the fact that I can't control DID is beside the point when it comes to personal responsibility. I don't believe my mental illness entitles me to some bad behavior or extra leniency. But just like I can't use DID as an excuse, neither can anyone else.
Dissociative Living
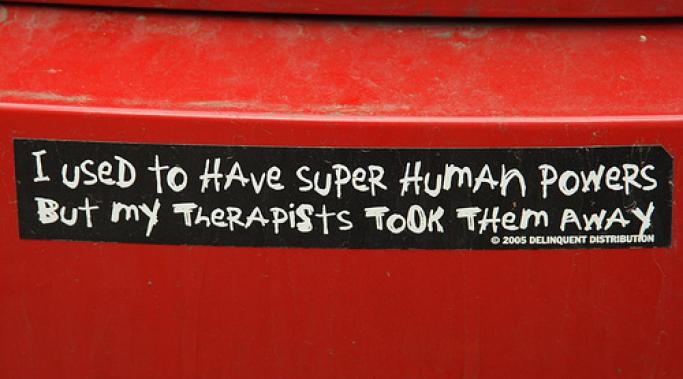
Last night I listened to the HealthyPlace Mental Health Radio Show interview with Sarah Olson, the author of Becoming One: A Story of Triumph Over Multiple Personality Disorder. She talked about her integration experience and I greedily took in every word. Here was someone who had achieved what was once my most fevered wish. After I got over the initial shock of my Dissociative Identity Disorder diagnosis, my focus narrowed to one elusive, coveted dream: the complete integration of alters. This shining promise of a cohesive, unified identity was all I wanted out of Dissociative Identity Disorder treatment.
My friend Dana recently moved to a new city and has searched fruitlessly for a therapist for months. Finding quality treatment for dissociative identity disorder (DID) is often one of the most frustrating challenges of living with DID. Despite the fascination it holds for many people, DID isn't widely understood, even among mental health professionals. Like so many others, Dana is in a position where she may have to choose between an inexperienced therapist and no therapist at all.
There's a disturbing trend in some Dissociative Identity Disorder support communities that has always turned me off. I call it the My Trauma Is Worse Than Your Trauma game. What starts as fellowship and camaraderie periodically deteriorates into an ugly rivalry among survivors of abuse. It's a competition that feeds off of and perpetuates the minimizing effects of child abuse.
I was sitting in a group therapy session once when the leader succinctly described the perception those of us with multiple personalities have of ourselves as groups of entirely separate people by writing the following on the white board: Me/Not Me. This is me. That is not me. For instance, I am a writer. But if another member of my system were assigned the task of writing this blog post, we would see how the Multiple Personality Disorder label came about. Some might have done a passable job. Others would have struggled mightily only to ultimately produce a choppy, thoroughly unimpressive piece of work. I am me. They are not me.
Yesterday I talked about the Dissociative Identity Disorder diagnosis and the vital role clinicians play in making that diagnosis. One of the reasons it's important to talk to a therapist if you think you may have DID is that dissociation by nature impedes awareness. Most people can't see the spot between their shoulder blades without a mirror. Similarly, most severely dissociative people aren't able to clearly recognize the symptoms of DID and the extent of their problem without the help of a skilled clinician. In fact, the diagnosis often comes as a shock. Today I'd like to share with you a typical diagnosis story - my own.
We were talking about dissociation when a man I once knew told me he'd been entirely unaware of a hospital stay until he got the bill. I didn't say it, but I immediately thought, 'he obviously has Dissociative Identity Disorder.' I now know how presumptuous that was. Though his experience was clearly indicative of something outside of everyday experience, it's taking a lot for granted to assume that something is DID. And looking back, it's absurd that I was so convinced. Not satisfied with a second opinion of my own diagnosis, I sought out four. One would think someone as hesitant to jump to conclusions as that would exercise a little more caution.
If you've ever seen a television crime show featuring a suspect with Dissociative Identity Disorder, you've seen a theatrical depiction of identity alteration, the fifth of the five main dissociative symptoms. A bewildered man suspected of murder is brought in for questioning. Eventually his manner, style of speech, and affect change dramatically and he says something like, "Sam didn't kill her. I did. I'm Joe." That switch in personality states is identity alteration at it's most extreme.
I used to make lists of things I liked and didn't like. If I wanted to marry and have children, that went on the list. If I enjoyed musical theater, that too went on the list. Inevitably a day would come when I couldn't imagine wanting to marry or liking musicals. I was perplexed as to why they were on the list in the first place. So I'd start a new one. I was trying hard to figure out who I was. As soon as I had a decent handle on the nature of my identity, it would slip through my fingers once again. I kept these lists in an effort to pin down my sense of self in a concrete and lasting way. What I didn't know is that I have Dissociative Identity Disorder. Identity confusion is a normal, if monumentally frustrating, part of DID.
We've covered depersonalization and derealization, two of the five core dissociative symptoms. As someone with dissociative identity disorder, both of those forms of dissociation affect me regularly. But the remaining three impact my life most profoundly. Dissociative amnesia, as I'll explain, is a deeply frustrating and disruptive part of living with DID.