Alternative Devices for Taking Insulin
Contents:
- What alternative devices for taking insulin are available?
- What are the prospects for an artificial pancreas?
- Points to Remember
- Hope through Research
- For More Information
- Acknowledgments

Many people with diabetes must take insulin to manage their disease.
Most people who take insulin use a needle and syringe to inject insulin just under the skin. Several other devices for taking insulin are available and new approaches are under development. No matter which approach a person uses for taking insulin, consistent monitoring of blood glucose levels is important. Good blood glucose control can prevent complications of diabetes.
What alternative devices for taking insulin are available?
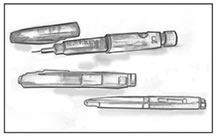
Insulin pens provide a convenient, easy-to-use way of injecting insulin and may be less painful than a standard needle and syringe. An insulin pen looks like a pen with a cartridge. Some of these devices use replaceable cartridges of insulin. Other pens are prefilled with insulin and are totally disposable after the insulin is injected. Insulin pen users screw a short, fine, disposable needle on the tip of the pen before an injection. Then users turn a dial to select the desired dose of insulin, inject the needle, and press a plunger on the end to deliver the insulin just under the skin. Insulin pens are less widely used in the United States than in many other countries.
Insulin pens are a convenient alternative to a needle and syringe for insulin injections.
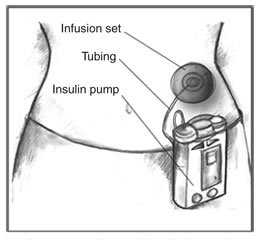
External insulin pumps are typically about the size of a deck of cards or cell phone, weigh about 3 ounces, and can be worn on a belt or carried in a pocket. Most pumps use a disposable plastic cartridge as an insulin reservoir. A needle and plunger are temporarily attached to the cartridge to allow the user to fill the cartridge with insulin from a vial. The user then removes the needle and plunger and loads the filled cartridge into the pump.
Insulin pumps contain enough insulin for several days. An infusion set carries insulin from the pump to the body through flexible plastic tubing and a soft tube or needle inserted under the skin.
Disposable infusion sets are used with insulin pumps to deliver insulin to an infusion site on the body, such as the abdomen. Infusion sets include a cannula—a needle or a small, soft tube—that the user inserts into the tissue beneath the skin. Devices are available to help insert the cannula. Narrow, flexible plastic tubing carries insulin from the pump to the infusion site. On the skin's surface, an adhesive patch or dressing holds the infusion set in place until the user replaces it after a few days.
Users set the pumps to give a steady trickle or "basal" amount of insulin continuously throughout the day. Pumps can also give "bolus" doses—one-time larger doses—of insulin at meals and at times when blood glucose is too high based on the programming set by the user. Frequent blood glucose monitoring is essential to determine insulin dosages and to ensure that insulin is delivered.

Injection ports provide an alternative to daily injections. Injection ports look like infusion sets without the long tubing. Like infusion sets, injection ports have a cannula that is inserted into the tissue beneath the skin. On the skin's surface, an adhesive patch or dressing holds the port in place. The user injects insulin through the port with a needle and syringe or an insulin pen. The port remains in place for several days and is then replaced. Use of an injection port allows a person to reduce the number of skin punctures to one every few days to apply a new port.
Using an injection port reduces the number of skin punctures to one every few days to apply a new port. The user injects insulin through the port.
Injection aids are devices that help users give injections with needles and syringes through the use of spring-loaded syringe holders or stabilizing guides. Many injection aids have a button the user pushes to inject the insulin.
Insulin jet injectors send a fine spray of insulin into the skin at high pressure instead of using a needle to deliver the insulin.
What are the prospects for an artificial pancreas?
To overcome the limitations of current insulin therapy, researchers have long sought to link glucose monitoring and insulin delivery by developing an artificial pancreas. An artificial pancreas is a system that will mimic, as closely as possible, the way a healthy pancreas detects changes in blood glucose levels and responds automatically to secrete appropriate amounts of insulin. Although not a cure, an artificial pancreas has the potential to significantly improve diabetes care and management and to reduce the burden of monitoring and managing blood glucose.
An artificial pancreas based on mechanical devices requires at least three components:
- a continuous glucose monitoring (CGM) system
- an insulin delivery system
- a computer program that adjusts insulin delivery based on changes in glucose levels
CGM systems approved by the U.S. Food and Drug Administration (FDA) include those made by Abbott, DexCom, and Medtronic. A CGM system paired with an insulin pump is available from Medtronic. This integrated system, called the MiniMed Paradigm REAL-Time System, is not an artificial pancreas, but it does represent the first step in joining glucose monitoring and insulin delivery systems using the most advanced technology available.
For more information about CGM systems, see the National Diabetes Information Clearinghouse's fact sheet Continuous Glucose Monitoring or call 1-800-860-8747 to request a copy.
Points to Remember
- Many people with diabetes who need insulin use a needle and syringe to inject insulin under the skin.
- The most common alternative ways to deliver insulin are insulin pens and insulin pumps. Injection ports, injection aids, and insulin jet injectors are also available.
- Researchers are developing an artificial pancreas, a system of mechanical devices that will automatically adjust insulin delivery based on changes in glucose levels.
- People who take insulin should monitor their blood glucose levels regularly.
- Good glucose control can prevent complications of diabetes.
Hope Through Research
Research supported by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Institutes of Health is contributing to the development of new technologies for continuous glucose monitoring, insulin delivery, and an artificial pancreas.
Participants in clinical trials can play a more active role in their own health care, gain access to new research treatments before they are widely available, and help others by contributing to medical research. For information about current studies, visit www.ClinicalTrials.gov.
For More Information
For more information about insulin and devices for taking insulin, see
- the publication What I need to know about Diabetes Medicines, available by calling 1-800-860-8747
- the FDA's information about insulin and insulin delivery devices at www.fda.gov/diabetes/insulin.html
- the American Diabetes Association's annual Resource Guide at www.diabetes.org/diabetes-forecast/resource-guide.jsp
Acknowledgments
Publications produced by the Clearinghouse are carefully reviewed by both NIDDK scientists and outside experts. This publication was reviewed by William V. Tamborlane, M.D., Yale University.
This publication may contain information about medications. When prepared, this publication included the most current information available. For updates or for questions about any medications, contact the U.S. Food and Drug Administration toll-free at 1-888-INFO-FDA (1-888-463-6332) or visit www.fda.gov. Consult your doctor for more information.
National Diabetes Education Program
1 Diabetes Way
Bethesda, MD 20814-9692
Internet: www.ndep.nih.gov
The National Diabetes Education Program is a federally funded program sponsored by the U.S. Department of Health and Human Services' National Institutes of Health and the Centers for Disease Control and Prevention and includes over 200 partners at the federal, state, and local levels, working together to reduce the morbidity and mortality associated with diabetes.
National Diabetes Information Clearinghouse
1 Information Way
Bethesda, MD 20892-3560
Internet: www.diabetes.niddk.nih.gov
The National Diabetes Information Clearinghouse (NDIC) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The NIDDK is part of the National Institutes of Health of the U.S. Department of Health and Human Services. Established in 1978, the Clearinghouse provides information about diabetes to people with diabetes and to their families, health care professionals, and the public. The NDIC answers inquiries, develops and distributes publications, and works closely with professional and patient organizations and Government agencies to coordinate resources about diabetes.
NIH Publication No. 09-4643
May 2009
APA Reference
Staff, H.
(2022, January 4). Alternative Devices for Taking Insulin, HealthyPlace. Retrieved
on 2025, November 2 from https://www.healthyplace.com/diabetes/treatments/alternative-devices-for-taking-insulin