What Are Opioid Drugs?
Thanks to the current opioid epidemic in the United States, many people are familiar with the term opioids. Further, many know that opioids are drugs, narcotics. Beyond the basics, there’s confusion about opioids meaning. Just what are opioid drugs, exactly?
Imagine a field that is an endless sea of delicate poppy flowers, mostly in reds and oranges but some in purples, blues, pinks, and whites. These beautiful poppies are part of the opium plant and are the origin of many opioid drugs. The well-known legal painkiller morphine is the active ingredient in the plant (Dovey, 2017).
Opioids, then, are drugs that can come from the poppy plant. While this is true, it’s not much of a definition. There’s more to opioids than meets the eye.
Opioids Meaning: Definition of Opioids
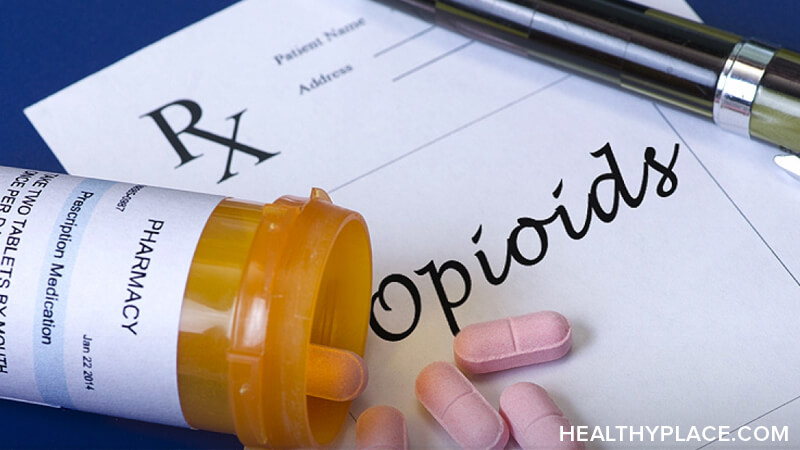
Opioids are painkillers you receive with a prescription. Opioids are illegal street drugs. Both types of drugs do the same thing in the body and brain.
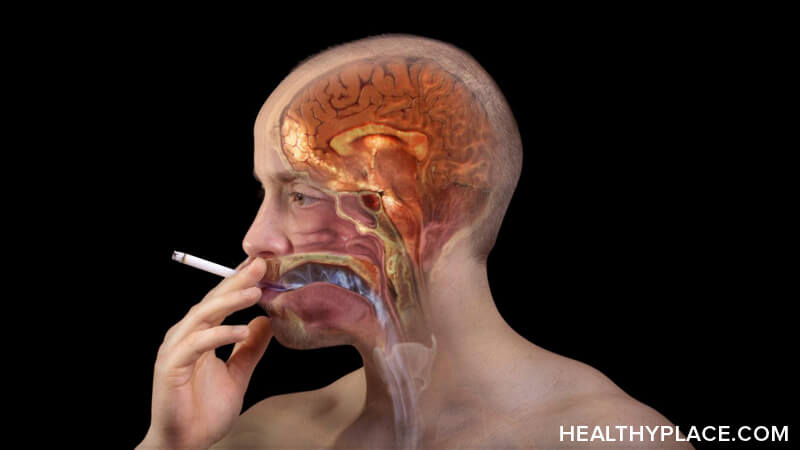
The brain and body have built-in opioid receptors, which are protein molecules, on the ends of some of the nerve cells throughout the central nervous system as well as the digestive tract. An opioid is any substance what will bind to these receptors and cause a response.
When an opioids drug—any opioid, prescription or street drug—and the opioids receptors attach, the result is what is often called the “opioid effect” (How Do Opioids Work? Mechanism of Action).
Opioids are a classification of sedative drugs that make people feel good. Opioid drugs in general:
- Increase the sensation of pleasure as pain is reduced
- Can induce euphoria, a feeling stronger than pleasure
- Are prescribed by doctors to reduce pain, both chronic pain and acute pain such as the pain that comes from medical procedures like surgery
- Are sold in illegal forms to people needing the high
- Have a strong potential to lead to dependence, overdose, and even death, and whether it’s heroin or a prescription painkiller like oxycodone, it can happen quickly (Opioids Deaths: Yes, Opioids Can Kill You)
Does a Drug Have To Be from the Opium Plant To Be an Opioid?
Opioid drugs can indeed be derived from poppies. It is from these plants that opiates external to the human body were first discovered by ancient civilizations, about 5,000 years ago. Many different opiates, including morphine, are natural alkaloids from the plant.
While the opium plant is the natural source of opioids, it doesn’t define an opioid because there are other sources, too. Some opioids, such as heroin, are semi-synthetic; which means they are man-made with ingredients derived from the opium plant. Others, like fentanyl, are fully synthetic and contain no naturally occurring opioid substance.
While there are different types of opioids derived from different sources, all have the same characteristic. An opioids drug is a highly addictive, sedative drug that binds to the body’s opioid receptors to reduce pain and heighten the experience of pleasure.
APA Reference
Peterson, T.
(2021, December 16). What Are Opioid Drugs?, HealthyPlace. Retrieved
on 2025, May 22 from https://www.healthyplace.com/addictions/opioid-addiction/what-are-opioid-drugs

 The United States is in the midst of an opioids epidemic. Beginning in the late 1990s and continuing thorough today, the nation has been in the throes of what “has been called the worst drug crisis in American history” (Nolan & Amilo, 2016).
The United States is in the midst of an opioids epidemic. Beginning in the late 1990s and continuing thorough today, the nation has been in the throes of what “has been called the worst drug crisis in American history” (Nolan & Amilo, 2016).