Opioids Deaths: Yes, Opioids Can Kill You
Opioids deaths are frighteningly common among people using any form of this drug. Opioids can cause death, and they do so much more easily that many people expect. It doesn’t matter what type of opioid someone is taking; all opioids can kill.
When people think of deadly opioid drugs, oftentimes they think of heroin. Heroin is a good drug to think about when trying to determine which drugs easily cause death. It’s incomplete, however. Prescription opioids—painkillers—are as easily lethal as their illegal counterparts. This is because all opioids work the same way in the brain and body. What they do in the body is why they are so deadly.
Opioids Deaths: How Opioids Can Kill You
Unfortunately, opioids deaths are common because many don’t understand how opioids work in the brain and body.
When someone takes a prescription painkiller or an illicit opioid drug, the opioids bond to specific opiate receptors in the brain and body. Not long after the person began using the opioid, his body stopped producing its own opioids, like endorphins. The body, then, was quickly dependent upon opioids. The body needed them to function, and if the person stops taking the opioid, he begins to experience opioids withdrawal symptoms.
The nature of opioids guarantees that dependence will happen, and many people who become dependent remain on opioids to avoid withdrawal. Further, especially in the case of prescription painkillers, they need legitimate pain management. These drugs are tricky things, though, and it’s very easy to develop a tolerance of opioids. This means that someone has to take more and more in order to get the same effect.
Opioids dependence often leads to opioid tolerance, which means that someone is taking increasingly high doses of the opioid. Opioids naturally slow down breathing, but when the dose is too high, the person experiences overdose (opioids toxicity). Breathing slows, becomes shallow, and stops. It is this opioids respiratory depression that is nearly always the cause of opioids death.
Opioids Respiratory Depression
Suppression of breathing is the deadliest aspect of opioids. It can happen to a first time user or someone who has been using opioids for years (and again, this applies to legally prescribed painkillers and illicit street drugs). Addiction is not required to die from opioids use. Opioids don’t discriminate. They’ll kill anyone.
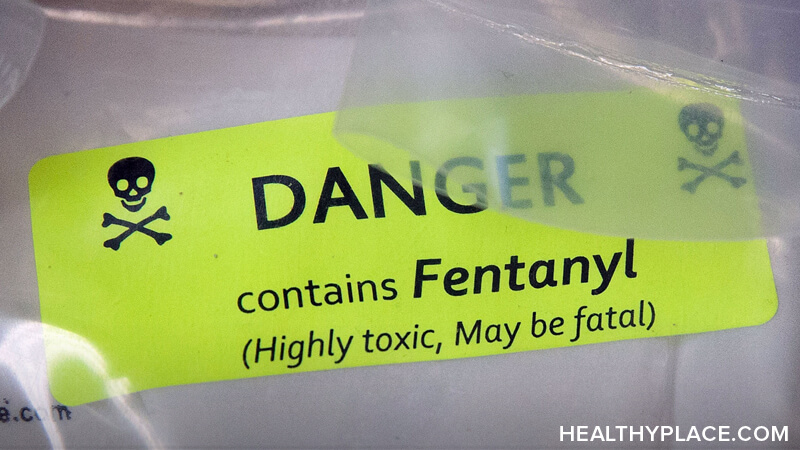
One other cause of opioids death, albeit on a much smaller scale than the opioid-induced respiratory depression that can happen to anyone using any opioid, is contaminants that are often found in heroin. Obviously, there are no regulations monitoring heroin production, and it’s often tainted with things like talc, quinine, and other poisons. However, the vast majority of opioids deaths come from an overdose that shuts down the respiratory system.
Opioids Deaths: How Often Do They Happen?
The statistics are staggering. A lot of people are dying from taking their prescribed painkillers, using someone else’s prescription painkillers, or from heroin and other illegal drugs. Here’s a look at some facts and figures that highlight the scope of the opioids epidemic:
- In less than 10 years (2006-2014), opioids overdose death rate rose 200% (Full House Committee on Oversight and Government Reform, 2016).
- In 2014, opioids deaths numbered 29,467 (10,574 of those were from heroin), while cocaine deaths numbered 5,415 (Nolan & Amilo, 2016).
- 16,651 opioids deaths happened in 2010 from prescription painkillers alone (Foreman, 2014).
- Approximately 78 Americans die every day from opioids overdose (Full House Committee on Oversight and Government Reform, 2016).
How opioids work in the body is a big reason for the opioids death rate. Another reason for the high number of deaths is that opioids are widely available and relatively easy to obtain. Yet another is that people are often unaware of the dangers of taking opioids. The more people know, the better they’ll be able to keep themselves safe. So yes, opioids can kill you. But they don’t have to.
APA Reference
Peterson, T.
(2021, December 16). Opioids Deaths: Yes, Opioids Can Kill You, HealthyPlace. Retrieved
on 2025, June 6 from https://www.healthyplace.com/addictions/opioid-addiction/opioids-deaths-yes-opioids-can-kill-you