Humalog for Treatment of Diabetes - Humalog Full Prescribing Information
Brand Names: Humalog Cartridge, Humalog KwikPen, Humalog Pen
Generic Name: Insulin Lispro
Dosage Form: Injection
Description
Pharmacology
Indications and Usage
Contraindications
Warnings
Precautions
Drug Interactions
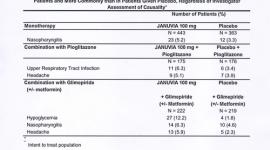
Adverse Reactions
Overdose
Dosage
Supplied
Humalog Pen, Humalog Cartridge, KwikPen, insulin lispro patient information (in plain English)
Description
Humalog® Mix75/25™ [75% insulin lispro protamine suspension and 25% insulin lispro injection, (rDNA origin)] is a mixture of insulin lispro solution, a rapid-acting blood glucose-lowering agent and insulin lispro protamine suspension, an intermediate-acting blood glucose-lowering agent. Chemically, insulin lispro is Lys(B28), Pro(B29) human insulin analog, created when the amino acids at positions 28 and 29 on the insulin B-chain are reversed. Insulin lispro is synthesized in a special non-pathogenic laboratory strain of Escherichia coli bacteria that has been genetically altered to produce insulin lispro. Insulin lispro protamine suspension (NPL component) is a suspension of crystals produced from combining insulin lispro and protamine sulfate under appropriate conditions for crystal formation.
Insulin lispro has the following primary structure:
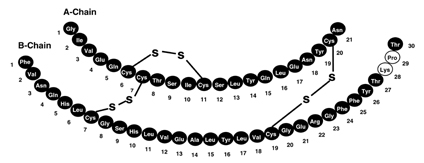
Insulin lispro has the empirical formula C257H383N65O77S6 and a molecular weight of 5808, both identical to that of human insulin.
Humalog Mix75/25 vials and Pens contain a sterile suspension of insulin lispro protamine suspension mixed with soluble insulin lispro for use as an injection.
Each milliliter of Humalog Mix75/25 injection contains insulin lispro 100 units, 0.28 mg protamine sulfate, 16 mg glycerin, 3.78 mg dibasic sodium phosphate, 1.76 mg Metacresol, zinc oxide content adjusted to provide 0.025 mg zinc ion, 0.715 mg phenol, and Water for Injection. Humalog Mix75/25 has a pH of 7.0 to 7.8. Hydrochloric acid 10% and/or sodium hydroxide 10% may have been added to adjust pH.
Clinical Pharmacology
Antidiabetic Activity
The primary activity of insulin, including Humalog Mix75/25, is the regulation of glucose metabolism. In addition, all insulins have several anabolic and anti-catabolic actions on many tissues in the body. In muscle and other tissues (except the brain), insulin causes rapid transport of glucose and amino acids intracellularly, promotes anabolism, and inhibits protein catabolism. In the liver, insulin promotes the uptake and storage of glucose in the form of glycogen, inhibits gluconeogenesis, and promotes the conversion of excess glucose into fat.
Insulin lispro, the rapid-acting component of Humalog Mix75/25, has been shown to be equipotent to Regular human insulin on a molar basis. One unit of Humalog® has the same glucose-lowering effect as one unit of Regular human insulin, but its effect is more rapid and of shorter duration. Humalog Mix75/25 has a similar glucose-lowering effect as compared with Humulin® 70/30 on a unit for unit basis.
Pharmacokinetics
Absorption
Studies in nondiabetic subjects and patients with type 1 (insulin-dependent) diabetes demonstrated that Humalog, the rapid-acting component of Humalog Mix75/25, is absorbed faster than Regular human insulin (U-100). In nondiabetic subjects given subcutaneous doses of Humalog ranging from 0.1 to 0.4 U/kg, peak serum concentrations were observed 30 to 90 minutes after dosing. When nondiabetic subjects received equivalent doses of Regular human insulin, peak insulin concentrations occurred between 50 to 120 minutes after dosing. Similar results were seen in patients with type 1 diabetes.
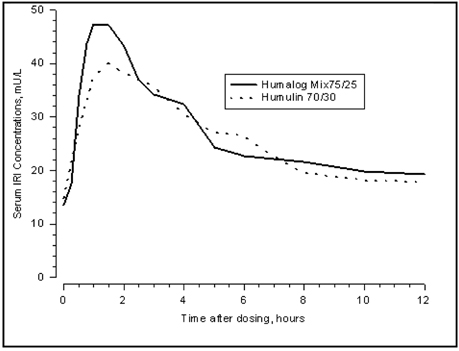
Figure 1: Serum Immunoreactive Insulin (IRI) Concentrations, After Subcutaneous Injection of Humalog Mix75/25 or Humulin 70/30 in Healthy Nondiabetic Subjects.
Humalog Mix75/25 has two phases of absorption. The early phase represents insulin lispro and its distinct characteristics of rapid onset. The late phase represents the prolonged action of insulin lispro protamine suspension. In 30 healthy nondiabetic subjects given subcutaneous doses (0.3 U/kg) of Humalog Mix75/25, peak serum concentrations were observed 30 to 240 minutes (median, 60 minutes) after dosing (see Figure 1). Identical results were found in patients with type 1 diabetes. The rapid absorption characteristics of Humalog are maintained with Humalog Mix75/25 (see Figure 1).
Figure 1 represents serum insulin concentration versus time curves of Humalog Mix75/25 and Humulin 70/30. Humalog Mix75/25 has a more rapid absorption than Humulin 70/30, which has been confirmed in patients with type 1 diabetes.
Distribution
Radiolabeled distribution studies of Humalog Mix75/25 have not been conducted. However, the volume of distribution following injection of Humalog is identical to that of Regular human insulin, with a range of 0.26 to 0.36 L/kg.
Metabolism
Human metabolism studies of Humalog Mix75/25 have not been conducted. Studies in animals indicate that the metabolism of Humalog, the rapid-acting component of Humalog Mix75/25, is identical to that of Regular human insulin.
Elimination
Humalog Mix75/25 has two absorption phases, a rapid and a prolonged phase, representative of the insulin lispro and insulin lispro protamine suspension components of the mixture. As with other intermediate-acting insulins, a meaningful terminal phase half-life cannot be calculated after administration of Humalog Mix75/25 because of the prolonged insulin lispro protamine suspension absorption.
Pharmacodynamics
Studies in nondiabetic subjects and patients with diabetes demonstrated that Humalog has a more rapid onset of glucose-lowering activity, an earlier peak for glucose-lowering, and a shorter duration of glucose-lowering activity than Regular human insulin. The early onset of activity of Humalog Mix75/25 is directly related to the rapid absorption of Humalog. The time course of action of insulin and insulin analogs, such as Humalog (and hence Humalog Mix75/25), may vary considerably in different individuals or within the same individual. The parameters of Humalog Mix75/25 activity (time of onset, peak time, and duration) as presented in Figures 2 and 3 should be considered only as general guidelines. The rate of insulin absorption and consequently the onset of activity is known to be affected by the site of injection, exercise, and other variables (see General under PRECAUTIONS).
In a glucose clamp study performed in 30 nondiabetic subjects, the onset of action and glucose-lowering activity of Humalog, Humalog® Mix50/50™, Humalog Mix75/25, and insulin lispro protamine suspension (NPL component) were compared (see Figure 2). Graphs of mean glucose infusion rate versus time showed a distinct insulin activity profile for each formulation. The rapid onset of glucose-lowering activity characteristic of Humalog was maintained in Humalog Mix75/25.
In separate glucose clamp studies performed in nondiabetic subjects, pharmacodynamics of Humalog Mix75/25 and Humulin 70/30 were assessed and are presented in Figure 3. Humalog Mix75/25 has a duration of activity similar to that of Humulin 70/30.
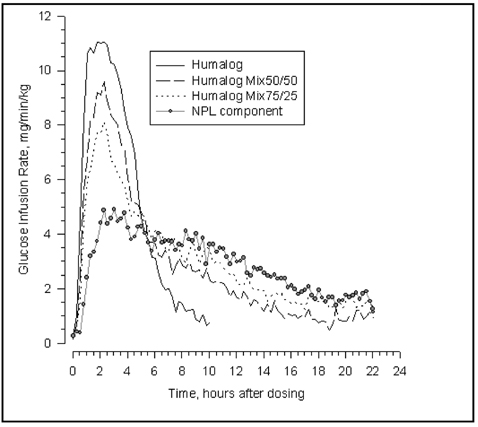
Figure 2: Insulin Activity After Injection of Humalog, Humalog Mix50/50, Humalog Mix75/25, or Insulin Lispro Protamine Suspension (NPL Component) in 30 Nondiabetic Subjects.
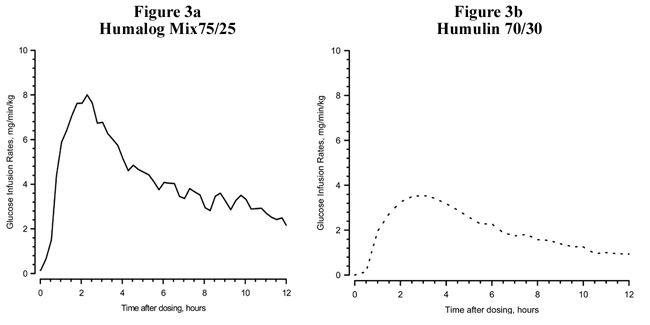
Figure 3: Insulin Activity After Injection of Humalog Mix75/25 and Humulin 70/30 in Nondiabetic Subjects.
Figures 2 and 3 represent insulin activity profiles as measured by glucose clamp studies in healthy nondiabetic subjects.
Figure 2 shows the time activity profiles of Humalog, Humalog Mix50/50, Humalog Mix75/25, and insulin lispro protamine suspension (NPL component).
Figure 3 is a comparison of the time activity profiles of Humalog Mix75/25 (see Figure 3a) and of Humulin 70/30 (see Figure 3b) from two different studies.
Special Populations
Age and Gender
Information on the effect of age on the pharmacokinetics of Humalog Mix75/25 is unavailable. Pharmacokinetic and pharmacodynamic comparisons between men and women administered Humalog Mix75/25 showed no gender differences. In large Humalog clinical trials, sub-group analysis based on age and gender demonstrated that differences between Humalog and Regular human insulin in postprandial glucose parameters are maintained across sub-groups.
Smoking
The effect of smoking on the pharmacokinetics and pharmacodynamics of Humalog Mix75/25 has not been studied.
Pregnancy
The effect of pregnancy on the pharmacokinetics and pharmacodynamics of Humalog Mix75/25 has not been studied.
Obesity
The effect of obesity and/or subcutaneous fat thickness on the pharmacokinetics and pharmacodynamics of Humalog Mix75/25 has not been studied. In large clinical trials, which included patients with Body Mass Index up to and including 35 kg/m2, no consistent differences were observed between Humalog and Humulin® R with respect to postprandial glucose parameters.
Renal Impairment
The effect of renal impairment on the pharmacokinetics and pharmacodynamics of Humalog Mix75/25 has not been studied. In a study of 25 patients with type 2 diabetes and a wide range of renal function, the pharmacokinetic differences between Humalog and Regular human insulin were generally maintained. However, the sensitivity of the patients to insulin did change, with an increased response to insulin as the renal function declined. Careful glucose monitoring and dose reductions of insulin, including Humalog Mix75/25, may be necessary in patients with renal dysfunction.
Hepatic Impairment
Some studies with human insulin have shown increased circulating levels of insulin in patients with hepatic failure. The effect of hepatic impairment on the pharmacokinetics and pharmacodynamics of Humalog Mix75/25 has not been studied. However, in a study of 22 patients with type 2 diabetes, impaired hepatic function did not affect the subcutaneous absorption or general disposition of Humalog when compared with patients with no history of hepatic dysfunction. In that study, Humalog maintained its more rapid absorption and elimination when compared with Regular human insulin. Careful glucose monitoring and dose adjustments of insulin, including Humalog Mix75/25, may be necessary in patients with hepatic dysfunction.
Indications and Usage
Humalog Mix75/25, a mixture of 75% insulin lispro protamine suspension and 25% insulin lispro injection, (rDNA origin), is indicated in the treatment of patients with diabetes mellitus for the control of hyperglycemia. Humalog Mix75/25 has a more rapid onset of glucose-lowering activity compared with Humulin 70/30 while having a similar duration of action. This profile is achieved by combining the rapid onset of Humalog with the intermediate action of insulin lispro protamine suspension.
Contraindications
Humalog Mix75/25 is contraindicated during episodes of hypoglycemia and in patients sensitive to insulin lispro or any of the excipients contained in the formulation.
Warnings
Humalog differs from Regular human insulin by its rapid onset of action as well as a shorter duration of activity. Therefore, the dose of Humalog Mix75/25 should be given within 15 minutes before a meal.
Hypoglycemia is the most common adverse effect associated with the use of insulins, including Humalog Mix75/25. As with all insulins, the timing of hypoglycemia may differ among various insulin formulations. Glucose monitoring is recommended for all patients with diabetes.
Any change of insulin should be made cautiously and only under medical supervision. Changes in insulin strength, manufacturer, type (e.g., Regular, NPH, analog), species, or method of manufacture may result in the need for a change in dosage.
Precautions
General
Hypoglycemia and hypokalemia are among the potential clinical adverse effects associated with the use of all insulins. Because of differences in the action of Humalog Mix75/25 and other insulins, care should be taken in patients in whom such potential side effects might be clinically relevant (e.g., patients who are fasting, have autonomic neuropathy, or are using potassium-lowering drugs or patients taking drugs sensitive to serum potassium level). Lipodystrophy and hypersensitivity are among other potential clinical adverse effects associated with the use of all insulins.
As with all insulin preparations, the time course of Humalog Mix75/25 action may vary in different individuals or at different times in the same individual and is dependent on site of injection, blood supply, temperature, and physical activity.
Adjustment of dosage of any insulin may be necessary if patients change their physical activity or their usual meal plan. Insulin requirements may be altered during illness, emotional disturbances, or other stress.
Hypoglycemia — As with all insulin preparations, hypoglycemic reactions may be associated with the administration of Humalog Mix75/25. Rapid changes in serum glucose concentrations may induce symptoms of hypoglycemia in persons with diabetes, regardless of the glucose value. Early warning symptoms of hypoglycemia may be different or less pronounced under certain conditions, such as long duration of diabetes, diabetic nerve disease, use of medications such as beta-blockers, or intensified diabetes control.
Renal Impairment — As with other insulins, the requirements for Humalog Mix75/25 may be reduced in patients with renal impairment.
Hepatic Impairment — Although impaired hepatic function does not affect the absorption or disposition of Humalog, careful glucose monitoring and dose adjustments of insulin, including Humalog Mix75/25, may be necessary.
Allergy — Local Allergy — As with any insulin therapy, patients may experience redness, swelling, or itching at the site of injection. These minor reactions usually resolve in a few days to a few weeks. In some instances, these reactions may be related to factors other than insulin, such as irritants in the skin cleansing agent or poor injection technique.
Systemic Allergy — Less common, but potentially more serious, is generalized allergy to insulin, which may cause rash (including pruritus) over the whole body, shortness of breath, wheezing, reduction in blood pressure, rapid pulse, or sweating. Severe cases of generalized allergy, including anaphylactic reaction, may be life threatening. Localized reactions and generalized myalgias have been reported with the use of cresol as an injectable excipient.
Antibody Production — In clinical trials, antibodies that cross-react with human insulin and insulin lispro were observed in both human insulin mixtures and insulin lispro mixtures treatment groups.
Information for Patients
Patients should be informed of the potential risks and advantages of Humalog Mix75/25 and alternative therapies. Patients should not mix Humalog Mix75/25 with any other insulin. They should also be informed about the importance of proper insulin storage, injection technique, timing of dosage, adherence to meal planning, regular physical activity, regular blood glucose monitoring, periodic hemoglobin A1c testing, recognition and management of hypo- and hyperglycemia, and periodic assessment for diabetes complications.
Patients should be advised to inform their physician if they are pregnant or intend to become pregnant.
Refer patients to the Patient Information leaflet for information on normal appearance, timing of dosing (within 15 minutes before a meal), storing, and common adverse effects.
For Patients Using Insulin Pen Delivery Devices: Before starting therapy, patients should read the Patient Information leaflet that accompanies the drug product and the User Manual that accompanies the delivery device and re-read them each time the prescription is renewed. Patients should be instructed on how to properly use the delivery device, prime the Pen to a stream of insulin, and properly dispose of needles. Patients should be advised not to share their Pens with others.
Laboratory Tests
As with all insulins, the therapeutic response to Humalog Mix75/25 should be monitored by periodic blood glucose tests. Periodic measurement of hemoglobin A1c is recommended for the monitoring of long-term glycemic control.
Drug Interactions
Insulin requirements may be increased by medications with hyperglycemic activity such as corticosteroids, isoniazid, certain lipid-lowering drugs (e.g., niacin), estrogens, oral contraceptives, phenothiazines, and thyroid replacement therapy.
Insulin requirements may be decreased in the presence of drugs that increase insulin sensitivity or have hypoglycemic activity, such as oral antidiabetic agents, salicylates, sulfa antibiotics, certain antidepressants (monoamine oxidase inhibitors), angiotensin-converting-enzyme inhibitors, angiotensin II receptor blocking agents, beta-adrenergic blockers, inhibitors of pancreatic function (e.g., octreotide), and alcohol. Beta-adrenergic blockers may mask the symptoms of hypoglycemia in some patients.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of Humalog, Humalog Mix75/25, or Humalog Mix50/50. Insulin lispro was not mutagenic in a battery of in vitro and in vivo genetic toxicity assays (bacterial mutation tests, unscheduled DNA synthesis, mouse lymphoma assay, chromosomal aberration tests, and a micronucleus test). There is no evidence from animal studies of impairment of fertility induced by insulin lispro.
Pregnancy
Teratogenic Effects — Pregnancy Category B
Reproduction studies with insulin lispro have been performed in pregnant rats and rabbits at parenteral doses up to 4 and 0.3 times, respectively, the average human dose (40 units/day) based on body surface area. The results have revealed no evidence of impaired fertility or harm to the fetus due to insulin lispro. There are, however, no adequate and well-controlled studies with Humalog, Humalog Mix75/25, or Humalog Mix50/50 in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
It is unknown whether insulin lispro is excreted in significant amounts in human milk. Many drugs, including human insulin, are excreted in human milk. For this reason, caution should be exercised when Humalog Mix75/25 is administered to a nursing woman. Patients with diabetes who are lactating may require adjustments in Humalog Mix75/25 dose, meal plan, or both.
Pediatric Use
Safety and effectiveness of Humalog Mix75/25 in patients less than 18 years of age have not been established.
Geriatric Use
Clinical studies of Humalog Mix75/25 did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently than younger patients. In general, dose selection for an elderly patient should take into consideration the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy in this population.
Adverse Reactions
Clinical studies comparing Humalog Mix75/25 with human insulin mixtures did not demonstrate a difference in frequency of adverse events between the two treatments.
Adverse events commonly associated with human insulin therapy include the following:
Body as a Whole — allergic reactions (see PRECAUTIONS).
Skin and Appendages — injection site reaction, lipodystrophy, pruritus, rash.
Other — hypoglycemia (see WARNINGS and PRECAUTIONS).
Overdose
Hypoglycemia may occur as a result of an excess of insulin relative to food intake, energy expenditure, or both. Mild episodes of hypoglycemia usually can be treated with oral glucose. Adjustments in drug dosage, meal patterns, or exercise, may be needed. More severe episodes with coma, seizure, or neurologic impairment may be treated with intramuscular/subcutaneous glucagon or concentrated intravenous glucose. Sustained carbohydrate intake and observation may be necessary because hypoglycemia may recur after apparent clinical recovery
Dosage and Administration
Table 1*: Summary of Pharmacodynamic Properties of Insulin Products (Pooled Cross-Study Comparison)
| |||
| Insulin Products | Dose, U/kg | Time of Peak Activity, Hours After Dosing | Percent of Total Activity Occurring in the First 4 Hours |
| Humalog | 0.3 | 2.4 | 70% |
| Humulin R | 0.32 | 4.4 | 54% |
| Humalog Mix75/25 | 0.3 | 2.6 | 35% |
| Humulin 70/30 | 0.3 | 4.4 | 32% |
| Humalog Mix50/50 | 0.3 | 2.3 | 45% |
| Humulin 50/50 | 0.3 | 3.3 | 44% |
| NPH | 0.32 | 5.5 | 14% |
| NPL component | 0.3 | 5.8 | 22% |
Humalog Mix75/25 is intended only for subcutaneous administration. Humalog Mix75/25 should not be administered intravenously. Dosage regimens of Humalog Mix75/25 will vary among patients and should be determined by the healthcare provider familiar with the patient's metabolic needs, eating habits, and other lifestyle variables. Humalog has been shown to be equipotent to Regular human insulin on a molar basis. One unit of Humalog has the same glucose-lowering effect as one unit of Regular human insulin, but its effect is more rapid and of shorter duration. Humalog Mix75/25 has a similar glucose-lowering effect as compared with Humulin 70/30 on a unit for unit basis. The quicker glucose-lowering effect of Humalog is related to the more rapid absorption rate of insulin lispro from subcutaneous tissue.
Humalog Mix75/25 starts lowering blood glucose more quickly than Regular human insulin, allowing for convenient dosing immediately before a meal (within 15 minutes). In contrast, mixtures containing Regular human insulin should be given 30 to 60 minutes before a meal.
The rate of insulin absorption and consequently the onset of activity are known to be affected by the site of injection, exercise, and other variables. As with all insulin preparations, the time course of action of Humalog Mix75/25 may vary considerably in different individuals or within the same individual. Patients must be educated to use proper injection techniques.
Humalog Mix75/25 should be inspected visually before use. Humalog Mix75/25 should be used only if it appears uniformly cloudy after mixing. Humalog Mix75/25 should not be used after its expiration date.
How Supplied
Humalog Mix75/25 [75% insulin lispro protamine suspension and 25% insulin lispro injection, (rDNA origin)] is available in the following package sizes: each presentation containing 100 units insulin lispro per mL (U-100).
| 10 mL vials | NDC 0002-7511-01 (VL-7511) |
| 5 x 3 mL prefilled insulin delivery devices (Pen) | NDC 0002-8794-59 (HP-8794) |
| 5 x 3 mL prefilled insulin delivery devices (KwikPen™) | NDC 0002-8797-59 (HP-8797) |
Storage — Humalog Mix75/25 should be stored in a refrigerator [2° to 8°C (36° to 46°F)], but not in the freezer. Do not use Humalog Mix75/25 if it has been frozen. Unrefrigerated [below 30°C (86°F)] vials must be used within 28 days or be discarded, even if they still contain Humalog Mix75/25. Unrefrigerated [below 30°C (86°F)] Pens, and KwikPens must be used within 10 days or be discarded, even if they still contain Humalog Mix75/25. Protect from direct heat and light. See table below:
| Not In-Use (Unopened) Room Temperature [Below 30°C (86°F)] | Not In-Use (Unopened) Refrigerated | In-Use (Opened) Room Temperature [Below 30°C (86°F)] | |
| 10 mL Vial | 28 days | Until expiration date | 28 days, refrigerated/room temperature. |
| 3 mL Pen and KwikPen (prefilled) | 10 days | Until expiration date | 10 days. Do not refrigerate. |
KwikPens manufactured by Eli Lilly and Company, Indianapolis, IN 46285, USA
Pens manufactured by Eli Lilly and Company, Indianapolis, IN 46285, USA or Lilly France, F-67640 Fegersheim, France
Vials manufactured byEli Lilly and Company, Indianapolis, IN 46285, USA or Lilly France, F-67640 Fegersheim, Francefor Eli Lilly and Company, Indianapolis, IN 46285, USA
www.Humalog.com
PV 5551 AMP
last updated 03/2009
Humalog Pen, Humalog Cartridge, KwikPen, insulin lispro patient information (in plain English)
Detailed Info on Signs, Symptoms, Causes, Treatments of Diabetes
The information in this monograph is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects. This information is generalized and is not intended as specific medical advice. If you have questions about the medicines you are taking or would like more information, check with your doctor, pharmacist, or nurse.
back to: Browse all Medications for Diabetes
APA Reference
Staff, H.
(2009, March 16). Humalog for Treatment of Diabetes - Humalog Full Prescribing Information, HealthyPlace. Retrieved
on 2026, March 1 from https://www.healthyplace.com/diabetes/medications/insulin-injecting-diabetes-treatment