There's a direct link between diabetes and erectile dysfunction (ED). Find out about the causes and treatments of diabetes erectile dysfunction.
Between 35 and 50 percent of men with diabetes will experience erectile dysfunction. It can be a complication of diabetes. There are, however, men that have diabetes and don't experience any sexual dysfunction.
Compared to men without diabetes, diabetic men tend to develop erectile dysfunction 10 to 15 years earlier. As these diabetic men get older, erectile dysfunction becomes even more common. At age 50+, 50-60% of these men with diabetes are likely to experience erection problems. Above age 70, there is about a 95% likelihood of having some difficulty with erectile function.
Causes of Erectile Dysfunction in Men with Diabetes
For men with diabetes, the causes of erectile dysfunction involve impairments in nerve, blood vessel and muscle function.
To get an erection, men need healthy blood vessels, nerves, male hormones, and a desire to be sexually stimulated. Diabetes can damage the blood vessels and nerves that control erection. Therefore, even if you have normal amounts of male hormones and you have the desire to have sex, you still may not be able to achieve a firm erection.
Contents:
Erectile dysfunction, sometimes called "impotence," is the repeated inability to get or keep an erection firm enough for sexual intercourse. The word "impotence" may also be used to describe other problems that interfere with sexual intercourse and reproduction, such as lack of sexual desire and problems with ejaculation or orgasm. Using the term erectile dysfunction makes it clear that those other problems are not involved.
Erectile dysfunction, or ED, can be a total inability to achieve erection, an inconsistent ability to do so, or a tendency to sustain only brief erections. These variations make defining ED and estimating its incidence difficult. Estimates range from 15 million to 30 million, depending on the definition used. According to the National Ambulatory Medical Care Survey (NAMCS), for every 1,000 men in the United States, 7.7 physician office visits were made for ED in 1985. By 1999, that rate had nearly tripled to 22.3. The increase happened gradually, presumably as treatments such as vacuum devices and injectable drugs became more widely available and discussing erectile function became accepted. Perhaps the most publicized advance was the introduction of the oral drug sildenafil citrate (Viagra) in March 1998. NAMCS data on new drugs show an estimated 2.6 million mentions of Viagra at physician office visits in 1999, and one-third of those mentions occurred during visits for a diagnosis other than ED.
In older men, ED usually has a physical cause, such as disease, injury, or side effects of drugs. Any disorder, like diabetes, that causes injury to the nerves or impairs blood flow in the penis has the potential to cause ED. Incidence increases with age: About 5 percent of 40-year-old men and between 15 and 25 percent of 65-year-old men experience ED. But it is not an inevitable part of aging.
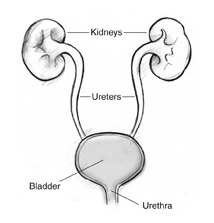
ED is treatable at any age, and awareness of this fact has been growing. More men have been seeking help and returning to normal sexual activity because of improved, successful treatments for ED. Urologists, who specialize in problems of the urinary tract, have traditionally treated ED; however, urologists accounted for only 25 percent of Viagra mentions in 1999.
How does an erection occur?
The penis contains two chambers called the corpora cavernosa, which run the length of the organ (see figure 1). A spongy tissue fills the chambers. The corpora cavernosa are surrounded by a membrane, called the tunica albuginea. The spongy tissue contains smooth muscles, fibrous tissues, spaces, veins, and arteries. The urethra, which is the channel for urine and ejaculate, runs along the underside of the corpora cavernosa and is surrounded by the corpus spongiosum.
Erection begins with sensory or mental stimulation, or both. Impulses from the brain and local nerves cause the muscles of the corpora cavernosa to relax, allowing blood to flow in and fill the spaces. The blood creates pressure in the corpora cavernosa, making the penis expand. The tunica albuginea helps trap the blood in the corpora cavernosa, thereby sustaining erection. When muscles in the penis contract to stop the inflow of blood and open outflow channels, erection is reversed.
Figure 1. Arteries (top) and veins (bottom) penetrate the long, filled cavities running the length of the penis—the corpora cavernosa and the corpus spongiosum. Erection occurs when relaxed muscles allow the corpora cavernosa to fill with excess blood fed by the arteries, while drainage of blood through the veins is blocked.
What causes erectile dysfunction (ED)?
Since an erection requires a precise sequence of events, ED can occur when any of the events is disrupted. The sequence includes nerve impulses in the brain, spinal column, and area around the penis, and response in muscles, fibrous tissues, veins, and arteries in and near the corpora cavernosa.
Damage to nerves, arteries, smooth muscles, and fibrous tissues, often as a result of disease, is the most common cause of ED. Diseases—such as diabetes, kidney disease, chronic alcoholism, multiple sclerosis, atherosclerosis, vascular disease, and neurologic disease—account for about 70 percent of ED cases. Between 35 and 50 percent of men with diabetes experience ED.
Lifestyle choices that contribute to heart disease and vascular problems also raise the risk of erectile dysfunction. Smoking, being overweight, and avoiding exercise are possible causes of ED.
Also, surgery (especially radical prostate and bladder surgery for cancer) can injure nerves and arteries near the penis, causing ED. Injury to the penis, spinal cord, prostate, bladder, and pelvis can lead to ED by harming nerves, smooth muscles, arteries, and fibrous tissues of the corpora cavernosa.
In addition, many common medicines—blood pressure drugs, antihistamines, antidepressants, tranquilizers, appetite suppressants, and cimetidine (an ulcer drug)—can produce ED as a side effect.
Experts believe that psychological factors such as stress, anxiety, guilt, depression, low self-esteem, and fear of sexual failure cause 10 to 20 percent of ED cases. Men with a physical cause for ED frequently experience the same sort of psychological reactions (stress, anxiety, guilt, depression). Other possible causes are smoking, which affects blood flow in veins and arteries, and hormonal abnormalities, such as not enough testosterone.
How is ED diagnosed?
Patient History
Medical and sexual histories help define the degree and nature of ED. A medical history can disclose diseases that lead to ED, while a simple recounting of sexual activity might distinguish among problems with sexual desire, erection, ejaculation, or orgasm.
Using certain prescription or illegal drugs can suggest a chemical cause, since drug effects account for 25 percent of ED cases. Cutting back on or substituting certain medications can often alleviate the problem.
Physical Examination
A physical examination can give clues to systemic problems. For example, if the penis is not sensitive to touching, a problem in the nervous system may be the cause. Abnormal secondary sex characteristics, such as hair pattern or breast enlargement, can point to hormonal problems, which would mean that the endocrine system is involved. The examiner might discover a circulatory problem by observing decreased pulses in the wrist or ankles. And unusual characteristics of the penis itself could suggest the source of the problem—for example, a penis that bends or curves when erect could be the result of Peyronie's disease.
Laboratory Tests
Several laboratory tests can help diagnose ED. Tests for systemic diseases include blood counts, urinalysis, lipid profile, and measurements of creatinine and liver enzymes. Measuring the amount of free testosterone in the blood can yield information about problems with the endocrine system and is indicated especially in patients with decreased sexual desire.
Other Tests
Monitoring erections that occur during sleep (nocturnal penile tumescence) can help rule out certain psychological causes of ED. Healthy men have involuntary erections during sleep. If nocturnal erections do not occur, then ED is likely to have a physical rather than psychological cause. Tests of nocturnal erections are not completely reliable, however. Scientists have not standardized such tests and have not determined when they should be applied for best results.
Psychosocial Examination
A psychosocial examination, using an interview and a questionnaire, reveals psychological factors. A man's sexual partner may also be interviewed to determine expectations and perceptions during sexual intercourse.
How is erectile dysfunction treated?
Most physicians suggest that treatments proceed from least to most invasive. For some men, making a few healthy lifestyle changes may solve the problem. Quitting smoking, losing excess weight, and increasing physical activity may help some men regain sexual function.
Cutting back on any drugs with harmful side effects is considered next. For example, drugs for high blood pressure work in different ways. If you think a particular drug is causing problems with erection, tell your doctor and ask whether you can try a different class of blood pressure medicine.
Psychotherapy and behavior modifications in selected patients are considered next if indicated, followed by oral or locally injected drugs, vacuum devices, and surgically implanted devices. In rare cases, surgery involving veins or arteries may be considered.
Psychotherapy
Experts often treat psychologically based ED using techniques that decrease the anxiety associated with intercourse. The patient's partner can help with the techniques, which include gradual development of intimacy and stimulation. Such techniques also can help relieve anxiety when ED from physical causes is being treated.
Drug Therapy
Drugs for treating ED can be taken orally, injected directly into the penis, or inserted into the urethra at the tip of the penis. In March 1998, the Food and Drug Administration (FDA) approved Viagra, the first pill to treat ED. Since that time, and tadalafil (Cialis) have also been approved. Additional oral medicines are being tested for safety and effectiveness.
Viagra, Levitra, and Cialis all belong to a class of drugs called phosphodiesterase (PDE) inhibitors. Taken an hour before sexual activity, these drugs work by enhancing the effects of nitric oxide, a chemical that relaxes smooth muscles in the penis during sexual stimulation and allows increased blood flow.
While oral medicines improve the response to sexual stimulation, they do not trigger an automatic erection as injections do. The recommended dose for Viagra is 50 mg, and the physician may adjust this dose to 100 mg or 25 mg, depending on the patient. The recommended dose for either Levitra or Cialis is 10 mg, and the physician may adjust this dose to 20 mg if 10 mg is insufficient. A lower dose of 5 mg is available for patients who take other medicines or have conditions that may decrease the body's ability to use the drug. Levitra is also available in a 2.5 mg dose.
None of these PDE inhibitors should be used more than once a day. Men who take nitrate-based drugs such as nitroglycerin for heart problems should not use either drug because the combination can cause a sudden drop in blood pressure. Also, tell your doctor if you take any drugs called alpha-blockers, which are used to treat prostate enlargement or high blood pressure. Your doctor may need to adjust your ED prescription. Taking a PDE inhibitor and an alpha-blocker at the same time (within 4 hours) can cause a sudden drop in blood pressure.
Oral testosterone can reduce ED in some men with low levels of natural testosterone, but it is often ineffective and may cause liver damage. Patients also have claimed that other oral drugs—including yohimbine hydrochloride, dopamine and serotonin agonists, and trazodone—are effective, but the results of scientific studies to substantiate these claims have been inconsistent. Improvements observed following use of these drugs may be examples of the placebo effect, that is, a change that results simply from the patient's believing that an improvement will occur.
Many men achieve stronger erections by injecting drugs into the penis, causing it to become engorged with blood. Drugs such as papaverine hydrochloride, phentolamine, and alprostadil (marketed as Caverject) widen blood vessels. These drugs may create unwanted side effects, however, including persistent erection (known as priapism) and scarring. Nitroglycerin, a muscle relaxant, can sometimes enhance erection when rubbed on the penis.
A system for inserting a pellet of alprostadil into the urethra is marketed as Muse. The system uses a prefilled applicator to deliver the pellet about an inch deep into the urethra. An erection will begin within 8 to 10 minutes and may last 30 to 60 minutes. The most common side effects are aching in the penis, testicles, and area between the penis and rectum; warmth or burning sensation in the urethra; redness from increased blood flow to the penis; and minor urethral bleeding or spotting.
Research on drugs for treating ED is expanding rapidly. Patients should ask their doctor about the latest advances.
Vacuum Devices
 Mechanical vacuum devices cause erection by creating a partial vacuum, which draws blood into the penis, engorging and expanding it. The devices have three components: a plastic cylinder, into which the penis is placed; a pump, which draws air out of the cylinder; and an elastic band, which is placed around the base of the penis to maintain the erection after the cylinder is removed and during intercourse by preventing blood from flowing back into the body (see figure 2).
Mechanical vacuum devices cause erection by creating a partial vacuum, which draws blood into the penis, engorging and expanding it. The devices have three components: a plastic cylinder, into which the penis is placed; a pump, which draws air out of the cylinder; and an elastic band, which is placed around the base of the penis to maintain the erection after the cylinder is removed and during intercourse by preventing blood from flowing back into the body (see figure 2).
Figure 2. A vacuum-constrictor device causes an erection by creating a partial vacuum around the penis, which draws blood into the corpora cavernosa. Pictured here are the necessary components: (a) a plastic cylinder, which covers the penis; (b) a pump, which draws air out of the cylinder; and (c) an elastic ring, which, when fitted over the base of the penis, traps the blood and sustains the erection after the cylinder is removed.
One variation of the vacuum device involves a semirigid rubber sheath that is placed on the penis and remains there after erection is attained and during intercourse.
Surgery
Surgery usually has one of three goals:
- to implant a device that can cause the penis to become erect
- to reconstruct arteries to increase the flow of blood to the penis
- to block off veins that allow blood to leak from the penile tissues
Implanted devices, known as prostheses, can restore erection in many men with ED. Possible problems with implants include mechanical breakdown and infection, although mechanical problems have diminished in recent years because of technological advances.
Malleable implants usually consist of paired rods, which are inserted surgically into the corpora cavernosa. The user manually adjusts the position of the penis and, therefore, the rods. Adjustment does not affect the width or length of the penis.
Inflatable implants consist of paired cylinders, which are surgically inserted inside the penis and can be expanded using pressurized fluid (see figure 3). Tubes connect the cylinders to a fluid reservoir and a pump, which are also surgically implanted. The patient inflates the cylinders by pressing on the small pump, located under the skin in the scrotum. Inflatable implants can expand the length and width of the penis somewhat. They also leave the penis in a more natural state when not inflated.
Figure 3. With an inflatable implant, erection is produced by squeezing a small pump (a) implanted in a scrotum. The pump causes fluid to flow from a reservoir (b) residing in the lower pelvis to two cylinders (c) residing in the penis. The cylinders expand to create the erection.
Surgery to repair arteries can reduce ED caused by obstructions that block the flow of blood. The best candidates for such surgery are young men with discrete blockage of an artery because of an injury to the crotch or fracture of the pelvis. The procedure is almost never successful in older men with widespread blockage.
Surgery to veins that allow blood to leave the penis usually involves an opposite procedure—intentional blockage. Blocking off veins (ligation) can reduce the leakage of blood that diminishes the rigidity of the penis during erection. However, experts have raised questions about the long-term effectiveness of this procedure, and it is rarely done.
Hope through Research
Advances in suppositories, injectable medications, implants, and vacuum devices have expanded the options for men seeking treatment for ED. These advances have also helped increase the number of men seeking treatment. Gene therapy for ED is now being tested in several centers and may offer a long-lasting therapeutic approach for ED.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) sponsors programs aimed at understanding the causes of erectile dysfunction and finding treatments to reverse its effects. NIDDK's Division of Kidney, Urologic, and Hematologic Diseases supported the researchers who developed Viagra and continue to support basic research into the mechanisms of erection and the diseases that impair normal function at the cellular and molecular levels, including diabetes and high blood pressure.
Points to Remember
- Erectile dysfunction (ED) is the repeated inability to get or keep an erection firm enough for sexual intercourse.
- ED affects 15 to 30 million American men.
- ED usually has a physical cause.
- ED is treatable at all ages.
- Treatments include psychotherapy, drug therapy, vacuum devices, and surgery.
For More Information
American Urological Association (AUA)
1000 Corporate Boulevard
Linthicum, MD 21090
Internet: www.auanet.org and www.urologyhealth.org
AUA can refer you to a urologist in your area.
Source: NIH Publication No. 06-3923, December 2005







 Mechanical vacuum devices cause erection by creating a partial vacuum, which draws blood into the penis, engorging and expanding it. The devices have three components: a plastic cylinder, into which the penis is placed; a pump, which draws air out of the cylinder; and an elastic band, which is placed around the base of the penis to maintain the erection after the cylinder is removed and during intercourse by preventing blood from flowing back into the body (see figure 2).
Mechanical vacuum devices cause erection by creating a partial vacuum, which draws blood into the penis, engorging and expanding it. The devices have three components: a plastic cylinder, into which the penis is placed; a pump, which draws air out of the cylinder; and an elastic band, which is placed around the base of the penis to maintain the erection after the cylinder is removed and during intercourse by preventing blood from flowing back into the body (see figure 2).

 Follow the healthy eating plan that you and your doctor or dietitian have worked out.
Follow the healthy eating plan that you and your doctor or dietitian have worked out. Be active a total of 30 minutes most days. Ask your doctor what activities are best for you.
Be active a total of 30 minutes most days. Ask your doctor what activities are best for you. Take your medicines as directed.
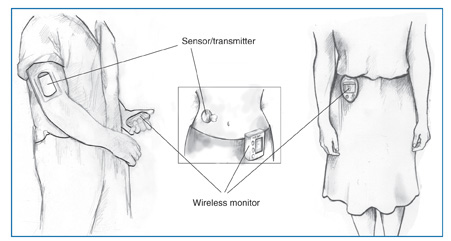
Take your medicines as directed. Check your blood glucose every day. Each time you check your blood glucose, write the number in your record book.
Check your blood glucose every day. Each time you check your blood glucose, write the number in your record book. Check your feet every day for cuts, blisters, sores, swelling, redness, or sore toenails.
Check your feet every day for cuts, blisters, sores, swelling, redness, or sore toenails. Brush and floss your teeth every day.
Brush and floss your teeth every day. Control your blood pressure and cholesterol.
Control your blood pressure and cholesterol. Don't smoke.
Don't smoke.